The Medic Guide serves as a comprehensive resource for medical professionals and individuals seeking reliable health information. It empowers users with practical advice and evidence-based insights.
1.1. Overview of the Medic Guide
The Medic Guide is a detailed resource designed to provide comprehensive medical knowledge. It covers essential topics, including emergency care, medical education, and patient communication. The guide serves as a bridge between theoretical knowledge and practical application, offering insights for healthcare professionals and individuals seeking medical information. It emphasizes evidence-based practices, ensuring accuracy and relevance in its content. Whether for education or reference, the Medic Guide is a valuable tool for understanding various aspects of healthcare, making it an indispensable resource for both professionals and patients.
1.2. Importance of a Comprehensive Medical Guide
A comprehensive medical guide is essential for ensuring accurate and accessible healthcare information. It standardizes medical knowledge, reducing errors and improving patient outcomes. For professionals, it serves as a reliable reference, aiding in diagnosis and treatment decisions. Patients benefit from clear, understandable content, empowering them to make informed choices. A well-structured guide also bridges gaps in emergency care and preventive medicine, ensuring preparedness and proactive health management. In an ever-evolving field, such a resource is vital for staying updated on best practices and advancements, making it indispensable for both healthcare providers and individuals seeking medical guidance.

Emergency Medical Care
Emergency medical care provides immediate assistance for acute illnesses or injuries, preventing complications and saving lives. It includes first aid, stabilization, and urgent interventions for conditions like cardiac arrest or trauma.
2.1. First Aid Basics
First aid basics are essential skills for immediate care of injuries or illnesses. They include assessing the situation, controlling bleeding, applying dressings, cleaning wounds, immobilizing fractures, and managing allergic reactions or cardiac arrests. Proper first aid prevents worsening conditions and saves lives. Key steps involve staying calm, calling for professional help when needed, and using available resources effectively. Understanding basic life support techniques, such as CPR, is crucial. Regular training ensures proficiency in these critical interventions, making everyone capable of providing timely assistance during emergencies.
2.2. Emergency Response Techniques
Emergency response techniques are critical for addressing life-threatening situations effectively. These methods include triage, rapid patient assessment, and the use of essential tools like automated external defibrillators (AEDs) and tourniquets. Proper training ensures prompt and accurate interventions, minimizing complications. Techniques such as airway management, bleeding control, and splinting fractures are vital. Staying calm and communicating clearly with the patient and team are equally important. Regular practice and updates on the latest protocols keep responders prepared for various emergencies, ensuring the best possible outcomes. These skills are indispensable in saving lives and stabilizing patients until professional medical help arrives.

Medical Education and Training
Medical education and training involve acquiring theoretical knowledge and practical skills to diagnose and treat patients effectively. Continuous learning and adaptation to advancements are crucial for professionals.
3.1. Choosing the Right Medical School
Choosing the right medical school is a pivotal decision that shapes your career. Consider factors like accreditation, curriculum, clinical opportunities, and faculty expertise. Research the school’s reputation, alumni success, and support systems. Location and cost are also critical; some schools offer scholarships or lower tuition. Assess the learning environment and student satisfaction. Ensure the program aligns with your career goals, whether in research, primary care, or specialties. Visit campuses if possible and connect with current students for insights. A well-rounded program with hands-on training and mentorship will provide a strong foundation for your medical journey.
3.2. Residency Programs and Specializations
Residency programs are crucial for refining medical skills and gaining practical experience. Choosing the right specialization requires careful consideration of personal interests, career goals, and patient demographics. Research the program’s curriculum, faculty expertise, and clinical opportunities. A strong application, including a compelling CV and personal statement, is essential for competitive specialties. Match algorithms and interviews play a significant role in placement. Residency also involves long hours and high-stakes decision-making, requiring resilience and adaptability. Building a supportive network and seeking mentorship can help navigate this challenging yet rewarding phase of medical training.

Medical Specializations
Medical specializations encompass diverse fields, each requiring unique expertise to address specific health needs. From surgery to pediatrics, these fields ensure comprehensive, specialized care for patients.
4.1. Overview of Popular Medical Fields
Popular medical fields include general practice, surgery, pediatrics, cardiology, and oncology. These specialties address a wide range of health conditions, ensuring comprehensive patient care. General practitioners provide primary care, while surgeons specialize in operative treatments. Pediatricians focus on children’s health, and cardiologists manage heart-related issues. Oncologists treat cancer, employing advanced therapies. Emerging fields like telemedicine and AI-driven medicine are transforming healthcare delivery. Each specialty requires unique expertise, enabling tailored treatment plans. This diversity ensures that patients receive specialized care, addressing their specific needs effectively.
4.2. Career Paths in Medicine
Medical careers offer diverse opportunities, from clinical practice to research and public health. After medical school, professionals can pursue residencies, fellowships, or specialized training. Physicians may choose private practice, academia, or hospital-based roles. Nurses and allied health professionals also have varied pathways. Public health experts focus on disease prevention, while researchers drive medical advancements. Administrative roles, such as healthcare management, are also viable. With evolving technologies like telemedicine, new career avenues emerge. Each path requires dedication and continuous learning, ensuring impactful contributions to patient care and healthcare development.
Advances in Medical Technology
Advances in medical technology integrate AI, telemedicine, and precision diagnostics, revolutionizing patient care and streamlining healthcare delivery for improved outcomes and accessibility.
5.1. Role of AI in Modern Medicine
AI significantly enhances modern medicine by improving diagnostic accuracy, streamlining clinical workflows, and enabling personalized treatment plans. AI algorithms analyze vast amounts of medical data, helping doctors identify patterns and predict patient outcomes more effectively. In imaging, AI aids in detecting abnormalities, reducing human error. Additionally, AI-powered chatbots assist patients with routine queries, freeing up healthcare providers for more critical tasks. AI also supports drug discovery, accelerating the development of new treatments. Its integration into healthcare systems has the potential to revolutionize patient care, making it more efficient and accessible while maintaining high standards of quality.
5.2. Telemedicine and Remote Care
Telemedicine has revolutionized healthcare by enabling remote consultations and monitoring, especially for patients with limited access to in-person care. Using video conferencing and mobile health apps, healthcare providers can diagnose and manage conditions remotely. This approach reduces hospital readmissions and improves chronic disease management. Telemedicine also enhances patient engagement by offering convenient follow-ups and mental health support. Despite its benefits, challenges like internet connectivity and data security remain. However, advancements in technology continue to expand telemedicine’s potential, making it a vital component of modern healthcare systems and improving overall patient outcomes globally.
Patient Care and Communication
Effective patient care and communication are cornerstone of healthcare. Clear dialogue, empathy, and trust build strong patient-provider relationships, leading to better health outcomes and a positive experience.
6.1. Building the Patient-Provider Relationship
Building a strong patient-provider relationship is foundational to effective care. It begins with active listening, empathy, and clear communication. Providers should foster trust by being approachable and transparent, ensuring patients feel heard and valued. Shared decision-making empowers patients, enhancing their engagement in care. Cultural sensitivity and understanding individual needs further strengthen the bond. Reliability and follow-through on commitments reinforce trust, while maintaining professional boundaries ensures a respectful dynamic. By prioritizing these elements, healthcare providers can create meaningful connections that improve patient satisfaction and outcomes. Effective communication and compassion are key to fostering lasting, therapeutic relationships.
6.2. Effective Communication Strategies
Effective communication is vital in healthcare, ensuring clarity and understanding between providers and patients. Active listening, clear language, and empathy are cornerstone strategies. Providers should avoid jargon, use plain language, and confirm comprehension; Non-verbal cues, such as eye contact and body language, reinforce trust. Regular updates and shared decision-making empower patients. Cultural competence and sensitivity to individual needs enhance interactions. Leveraging technology, like patient portals, can improve accessibility. Encouraging questions and addressing concerns promptly fosters a supportive environment. By tailoring communication to each patient’s preferences and literacy level, providers ensure meaningful engagement and better health outcomes. Effective strategies bridge gaps and strengthen care quality.

Legal and Ethical Considerations
Understanding legal and ethical standards is crucial in healthcare, addressing malpractice, patient confidentiality, and informed consent. These principles guide professionals in navigating complex medical and moral dilemmas effectively.
7.1. Medical Malpractice and Liability
Medical malpractice occurs when healthcare providers deviate from accepted standards, causing harm to patients. Liability often involves negligence, misdiagnosis, or surgical errors. Providers must carry malpractice insurance to protect against lawsuits and financial loss. Understanding malpractice laws is essential for both professionals and patients, ensuring accountability and fair compensation. Proper documentation and transparent communication can mitigate risks, fostering trust in the healthcare system. Staying informed about legal frameworks helps providers navigate challenges and maintain high standards of care.
7.2. Ethical Dilemmas in Healthcare
Ethical dilemmas in healthcare arise when professionals face conflicting moral obligations, such as maintaining patient confidentiality versus reporting harmful behavior. Issues like end-of-life care, resource allocation, and informed consent often challenge providers. These situations require careful consideration of ethical principles, such as autonomy, beneficence, and justice. Guidelines like the Hippocratic Oath and professional codes of conduct provide frameworks for decision-making. Open communication and empathy are crucial in resolving these dilemmas, ensuring respect for patient autonomy while upholding ethical standards. Addressing these challenges fosters trust and integrity in the healthcare system, benefiting both patients and providers.

Mental Health and Well-being
Mental health is vital for overall well-being, encompassing emotional, psychological, and social stability. Recognizing signs of stress and burnout is crucial for maintaining resilience and balance in life.
8.1. Managing Stress for Healthcare Professionals
Managing stress for healthcare professionals is essential to maintain their well-being and effectiveness. High-pressure environments can lead to burnout, impacting both personal health and patient care quality. Techniques such as mindfulness, time management, and seeking support from colleagues or mental health professionals can help alleviate stress. Regular breaks, self-care practices, and open communication within teams are also crucial; Employers should foster a supportive environment, encouraging work-life balance and providing resources for stress management. Addressing these factors ensures healthcare providers can thrive, delivering optimal care while safeguarding their mental health.
8.2. Burnout Prevention Strategies
Burnout prevention strategies are vital for maintaining the well-being of healthcare professionals. Recognizing early signs, such as emotional exhaustion or reduced performance, is crucial. Employing self-care practices, like regular exercise and mindfulness, can mitigate burnout. Organizations should promote a supportive work culture, offering flexible schedules and mental health resources. Encouraging open dialogue and fostering a sense of community among staff can also help. Providing opportunities for professional development and ensuring a healthy work-life balance are key. Proactive approaches, such as stress management workshops and access to counseling, further enhance burnout prevention. These strategies not only benefit individuals but also improve overall patient care quality.

Global Health Initiatives
Global health initiatives address disparities, improve access, and promote wellness worldwide. Collaborative efforts focus on disease prevention, education, and equitable care, ensuring healthier communities globally.
9.1. Public Health Challenges Worldwide
Public health challenges worldwide include infectious diseases, pandemics, and limited access to healthcare. Issues like vaccine distribution, malnutrition, and climate change exacerbate these problems. Conflicts disrupt health systems, leading to disease outbreaks. Mental health crises, rising chronic diseases, and antimicrobial resistance further strain global health efforts; Addressing these challenges requires collaboration, innovation, and equitable resource allocation to ensure sustainable solutions and improve global health outcomes.
9.2. Humanitarian Work in Medicine
Humanitarian work in medicine involves delivering healthcare to vulnerable populations during crises. Organizations like Médecins Sans Frontières provide aid in disaster zones and conflict areas. Volunteers face challenges like limited resources and safety risks while saving lives. Their efforts include training local staff and rebuilding healthcare systems. The emotional toll is high, but the impact is profound. Humanitarian medicine bridges gaps in global health, inspiring change and fostering resilience. It highlights the importance of compassion and solidarity in addressing health disparities worldwide, ensuring no one is left behind in times of need.

Pharmacology and Drug Development
Pharmacology explores medications’ effects and development processes. Understanding dosages, interactions, and clinical trials is crucial. Drug development involves extensive research, FDA approvals, and ensuring safety and efficacy for patients.
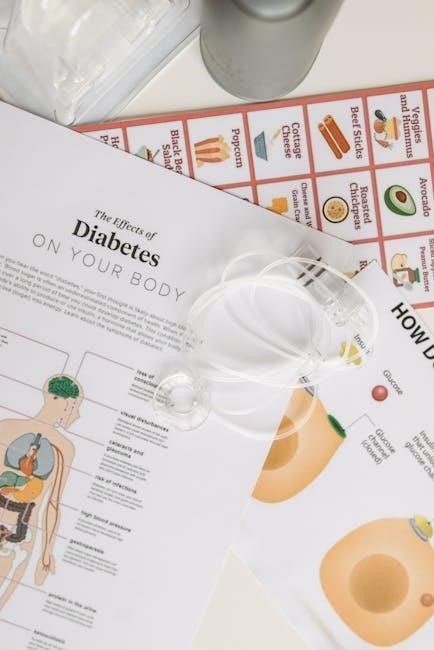
10.1. Understanding Medications and Dosages
Understanding medications and dosages is critical for safe and effective treatment. Medications are substances designed to diagnose, treat, or prevent diseases, while dosages refer to the amount and frequency of administration. Proper dosing ensures efficacy and minimizes risks of side effects or toxicity. Factors like age, weight, and health status influence dosing. Patients must adhere to prescribed regimens and be aware of potential interactions with other drugs or foods. Clear communication between healthcare providers and patients is essential to avoid errors and optimize therapeutic outcomes. This section provides insights into the fundamentals of pharmacology and safe medication practices for both professionals and patients.
10.2. Clinical Trials and Drug Approval
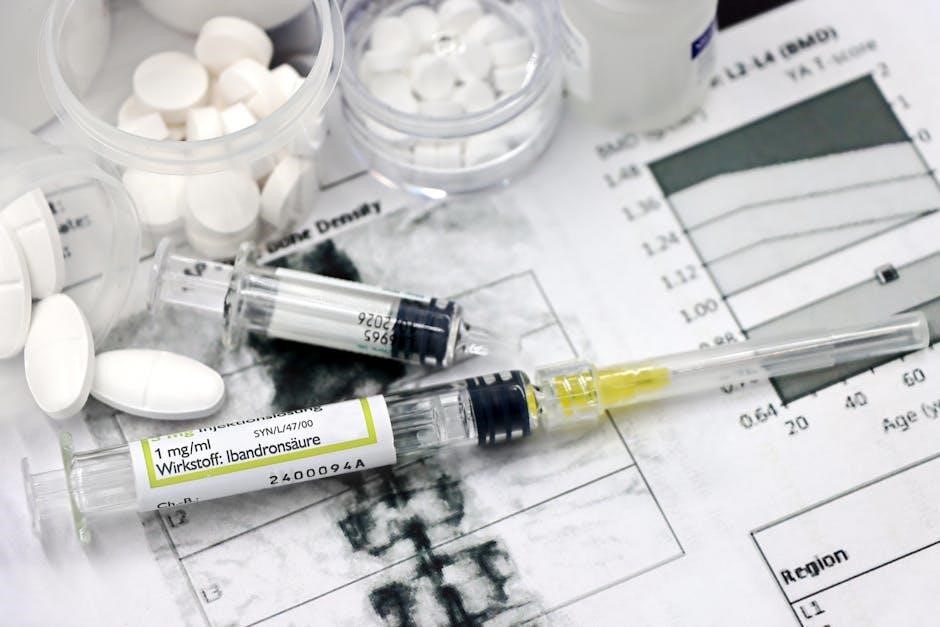
Clinical trials are a cornerstone of drug development, ensuring medications are safe and effective before they reach patients. These trials are conducted in phases, starting with small groups to assess safety and ending with large-scale studies to confirm efficacy. Regulatory bodies, such as the FDA, review trial data to grant approval. This rigorous process ensures that only drugs meeting strict safety and efficacy standards are marketed. Transparency and ethical practices are paramount to maintain public trust. Understanding the complexities of clinical trials and drug approval is essential for both healthcare professionals and patients seeking reliable treatments.
Healthcare Administration
Healthcare administration involves managing hospital operations, staffing, and resource allocation to ensure efficient workflows and high-quality patient care, supported by strategic planning and policy implementation, along with financial oversight and regulatory compliance.
11.1. Managing Hospital Operations
Managing hospital operations requires balancing patient care, resource allocation, and staff coordination. Effective leadership ensures smooth workflows, optimizing service delivery while maintaining quality and safety standards. Administrators oversee departments, implement policies, and monitor performance metrics to enhance efficiency. They also handle budgeting, supply chain management, and compliance with regulations. Strong communication and decision-making are critical to address challenges like staff shortages or equipment shortages. By integrating technology and fostering collaboration, hospitals can improve patient outcomes and overall operational excellence.
11.2. Healthcare Policy and Reform
Healthcare policy and reform shape the framework for delivering medical services, ensuring access, affordability, and quality. Governments and organizations develop regulations to address systemic challenges, such as rising costs and unequal access. Reforms often focus on expanding insurance coverage, reducing administrative burdens, and promoting preventive care. Advocacy groups and policymakers collaborate to create equitable solutions, while technological advancements and data-driven approaches enhance decision-making. Staying informed about policy changes is crucial for healthcare professionals and patients alike, as these reforms directly impact care delivery and outcomes.
The Medic Guide concludes by emphasizing the importance of adaptability and continuous education in the ever-evolving field of medicine. It encourages professionals to stay informed and dedicated to improving patient care and their own growth.
12.1. Final Thoughts on the Medic Guide
The Medic Guide has provided a vast array of insights into the medical field, offering practical advice and evidence-based knowledge. It emphasizes the importance of adaptability, continuous learning, and ethical practices in healthcare. By staying informed and proactive, professionals and individuals can navigate the complexities of medicine effectively. The guide serves as a foundation for understanding key concepts, from emergency care to advanced technologies, ensuring readers are well-equipped to make informed decisions. Ultimately, it encourages a commitment to excellence and compassion, fostering a culture of improvement and care in the ever-evolving world of medicine.
12.2. Continuous Learning in Medicine
Continuous learning is essential in medicine, as advancements in technology and research evolve rapidly. Professionals must stay updated on the latest treatments, ethical practices, and innovations like AI and telemedicine. Lifelong learning ensures adaptability and improved patient outcomes. By embracing educational resources and staying curious, healthcare providers can maintain excellence and navigate the ever-changing medical landscape effectively. This commitment to growth not only enhances professional competence but also fosters a culture of innovation and care, benefiting both individuals and the broader healthcare community.






